March 2025 Case
Authors
Jennifer Lee, MD (Fellow), Jing M. Zhai, MD, PhD (Faculty)
Cytopathology
ION navigated FNAC of a lung mass
Case Presentation
A 54-year-old man presented to the emergency department with persistent and worsening symptoms after being diagnosed with pneumonia at an outside facility, where outpatient antibiotic therapy failed. A PET-CT scan revealed a 1.1 cm irregular solid nodular opacity in the left lower lobe with low metabolic activity. The patient underwent ION navigation robotic- assisted bronchoscopic ultrasound-guided fine needle aspiration (FNA) of the left lower lobe lung, anterior segment nodule. Bronchoalveolar lavage and biopsies were also collected simultaneously.
Cytological Findings
The cytopathology department received 40 cc of needle rinse in CytoRich Red solution. The lab prepared one SurePath slide from the solution and processed the rest as a cell block. The SurePath slide and one cell block slide were evaluated, and additional special tests, including GMS and mucicarmine stains, were performed.
The specimen was composed of reactive bronchial cells, alveolar macrophages, mixed inflammatory cells, and foamy amorphous material. Oval to round refractile organisms with halos were observed. The cell block showed focal changes suggestive of ill-formed epithelioid granuloma. The GMS stain revealed larger Cryptococcus species and smaller Pneumocystis species. Mucicarmine stain highlighted the mucinous capsule of Cryptococcus.
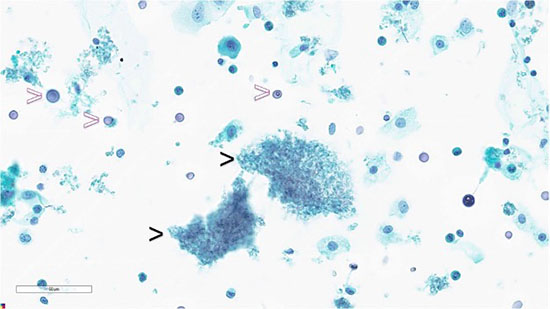
Figure 1: Lung FNA, SurePath, Papanicolaou stain: foamy amorphous materials (black arrowheads), and Cryptococcus organisms (white arrowheads).
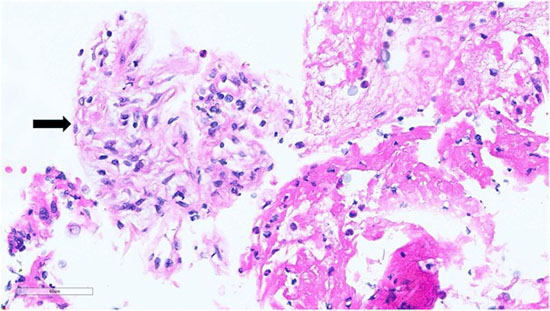
Figure 2: Lung FNA, Cell Block, Hematoxylin and eosin stain: epithelioid histiocytes and lymphocytes suggestive of ill-formed granuloma (black arrow)
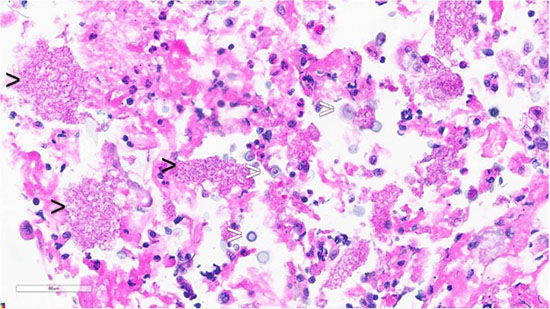
Figure 3: Lung FNA, Cell Block, Hematoxylin and eosin stain: foamy amorphous materials (black arrowheads), Cryptococcus organisms (white arrowheads), with histiocytes and lymphocytes.
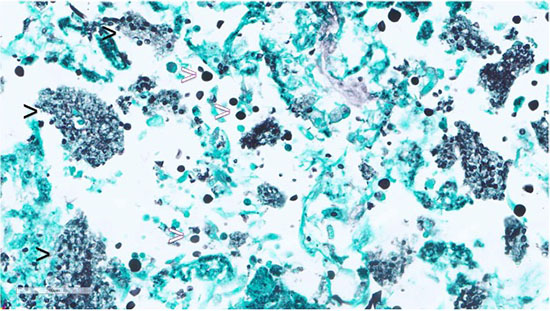
Figure 4: Lung FNA, Cell Block, GMS stain: highlights Pneumocystis jirovecii (black arrowheads) and Cryptococcus species (white arrowheads).
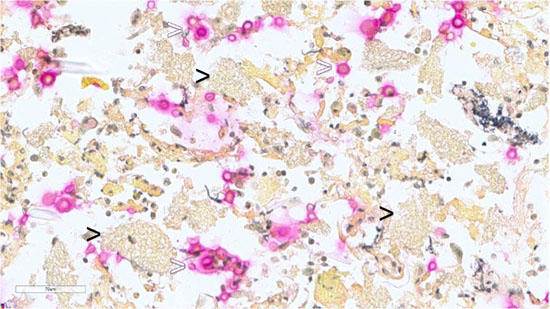
Figure 5: Lung FNA, Cell Block, Mucicarmine stain: highlights mucinous capsule of Cryptococcus species (white arrowheads) and negative in foamy amorphous materials (black arrowheads).
Diagnosis
The lung FNA was diagnosed as ill-formed granuloma with dual organisms consistent with Cryptococcus species and Pneumocystis jirovecii infection.
Discussion
The patient underwent a diagnostic procedure involving transbronchial FNA biopsy, cryobiopsy and bronchioalveolar lavage to investigate the pulmonary nodule. The presence of Pneumocystis was confirmed in all three specimens including FNA biopsy, cryobiopsy, and the bronchial lavage. Cryptococcus species infection was detected only in the FNA sample.
Following these findings, the patient was tested for HIV and was found to be positive. The presence of concurrent infection with Pneumocystis and Cryptococcus suggests that the patient may be experiencing immunosuppression, which is commonly associated with HIV infection.
Both infections could induce a non-necrotizing granulomatous inflammatory reaction and present as a mass-forming lesion. This diagnosis allows for appropriate management and treatment of the patient's condition, focusing on both the opportunistic infections and the underlying HIV infection.
P. jirovecii does not grow in vitro; hence, a definitive diagnosis requires the demonstration of cysts or trophozoites in lung tissue or respiratory specimens such as bronchoalveolar lavage. The cyst forms of P. jirovecii appear as thick-walled, approximately 5-8 µm round structures with up to eight intracystic bodies. Trophozoite forms are smaller pleomorphic structures with a size of 1-5 µm and contain a single nucleus. The organisms are not visible with Papanicolaou stains but appear as green, foamy alveolar casts. Grocott-methenamine silver stain is used to visualize the cyst form of P.jiroveci. Giemsa stain of air-dried smear is useful to identify the cystic form as negative images, and the intracystic bodies and trophozoite as blue dots. More advanced techniques such as immunofluorescence microscopy and molecular methods are available for higher sensitivity and specificity for the detection of the pathogen.
Cryptococcus organisms are narrow-based budding yeasts with variable sizes ranging from 4- 15 μm, with a thick mucin capsule, appearing as clear spaces around yeast cells in H&E stain. Diagnosis is crucial due to potential dissemination to the central nervous system, which has a high mortality rate. Mucicarmine and GMS stains are essential for diagnosing cryptococcosis. Fungal culture and MALDI-TOF MS are available for species identification.
Take-Home Message
Fine needle aspiration cytology provides critical pathological information in this case. When diagnosing an opportunistic infection, it is important to consider the possibility of concurrent infections, as some may only be identified through tissue examination. A thorough understanding of the morphology of different fungal organisms is essential for accurately detecting these coexisting infections. This case emphasizes the importance of multi-technique diagnosis in identifying complex opportunistic infections associated with HIV infection.
References
- Marina Vivero and Christopher A. French, Respiratory tract and mediastinum, Cytology 5th edition Cytology: Diagnostic Principles and Clinical Correlates, 2, 70-74
- Peter C. Iwen, George R. Thompson and Nathan P. Wiederhold. Mycotic Diseases, Henry's Clinical Diagnosis and Management by Laboratory Methods, Chapter 60, 1194-1228.e7
- Jeffrey L. Myers. Lung. (2018). In Rosai and Ackerman’s Surgical Pathology (11th ed.).
Elsevier, Chapter 3 (10), 380-395. - Centers for Disease Control and Prevention. (2017, December 30). CDC - dpdx - pneumocystis.
Centers for Disease Control and Prevention.
https://www.cdc.gov/dpdx/pneumocystis/index.html